Fungal infections in the brain aren’t just the stuff of movies – Africa grapples with a deadly epidemic

Rachael Dangarembizi, University of Cape Town
In the 2023 American post-apocalyptic drama television series The Last of Us, humans are plunged towards extinction as a fungal infection of the brain zombie-fies most of the species. This may seem far-fetched but fungi can, and do, infect human brains.
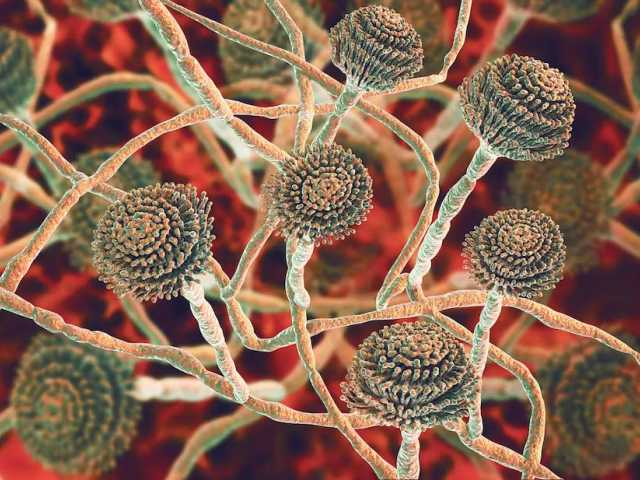
Fungi are present everywhere in our environment: in the air, in the soil, in decaying plant material, on our skin, and even in the gut as part of our natural flora.
Microscopic, disease-causing fungi can invade various parts of the body, leading to a range of symptoms and health problems. In fact, fungal infections contribute to about 1.5 million deaths every year.
I am a neurobiologist who has been studying fungal infections of the brain for 10 years. I was part of a team that recently published a review discussing the emergence, and re-emergence, of fungal infections in Africa, especially in sub-Saharan Africa. We conclude that Africa is suffering from a silent, but costly, epidemic of fungal infections. We found that the emergence of deadly fungal infections in the region is primarily driven by a high burden of HIV infections, lack of access to quality healthcare, and unavailability of effective antifungal drugs.
What are fungal infections?
For the greater part of the history of humankind, fungal infections were never a threat to human health. This is mainly because most fungi cannot survive the warm human body temperature of 37°C. However, climate change and other environmental pressures have led to the emergence of species of fungi that are capable of surviving at human body temperatures.
Even then, our immune systems are quite capable of fighting against fungal infections. For instance, our bodies can create localised acidic environments, limit micronutrient availability and release antimicrobial agents.
However, when the immune system is weakened, fungi are able to evade the body’s defences and avoid detection. They can generate bioactive agents which help them evade or adjust to the host immune response. Some adapt to survive in hostile, low-nutrient and low-oxygen environments.
Immunocompromised people are at risk of developing serious or life-threatening fungal diseases. Africa accounts for 67% of the global burden of HIV, and opportunistic fungal diseases are on the rise.
Some examples
One example of opportunistic fungal diseases is cryptococcal meningitis, which emerged with the HIV pandemic in the late 1980s. Today, sub-Saharan Africa contributes about 73% of all global cases and deaths resulting from the disease. Cryptococcal meningitis is caused by the fungus Cryptococcus neoformans, which is found in soil and bird droppings. Infection by the fungus occurs when someone inhales fungal spores. It first leads to the development of a lung infection and later a fatal brain infection. Cryptococcal meningitis is a leading cause of adult meningitis in sub-Saharan Africa and it’s associated with almost 20% of all AIDS-related deaths.
Effective treatments for cryptococcal meningitis are unaffordable and inaccessible for most affected people. Costs range between US$1,400 and US$2,500 per patient for a full two-week antifungal treatment course.
The development of cheaper drugs has been hindered by a limited understanding of how the fungus causes such extreme damage in the brain.
Another example of an HIV-related opportunistic fungal disease is pneumocystis jirovecii pneumonia. It’s caused by a ubiquitous, airborne fungus Pneumocystis jirovecii, which is passed on from person to person. Pneumocystis hardly causes trouble in people with healthy immune systems, but they act as reservoirs and pass the infection to those with poor immune systems, who may develop serious symptoms including fever, a dry cough and trouble with breathing. Pneumocystis jirovecii pneumonia occurs in 15%-20% of HIV patients who present with respiratory problems.
The diagnosis of pneumocystis jiroveci pneumonia is expensive and requires a well-equipped laboratory. In Africa’s poor urban and rural healthcare facilities this will be a challenge. The fungus, P. jirovecii, is also extremely difficult to culture, which limits diagnosis and research.
Growing burden
In our review, we found various factors driving the emergence and reemergence of fungal threats. They include climate change, the spread of immunosuppressive diseases, medical advances such as organ transplants (the immune system is suppressed to minimise rejection), the use of immunosuppressants to manage inflammatory diseases, and the use of antibiotics.
While these factors are not unique to Africa, the burden of fungal diseases and the number of people who succumb to them is much greater.
The COVID pandemic seems to have made the global fungal burden worse. For instance, recent studies have shown that people who were infected with COVID and have recovered are vulnerable to infection with a fungus called mucormycosis, also known as the black fungus. COVID-induced lung damage, high blood sugar, and the steroids often used to treat it are all predisposing factors to black fungus infection. With a reduced capacity to clear fungal spores and a reduced immune response, thanks to the steroids, the fungus can gain entry and infect the sinuses and facial bones, eventually moving to the brain.
But don’t we have antifungal drugs?
Most of the population affected by fungal infections live in rural or poor urban settlements.
With poorly funded and overburdened healthcare systems, many African countries are not well prepared to deal with fungal infections. Additionally, some of the WHO-recommended antifungal drugs – such as flucytosine – are unavailable in most African countries. Ineffective and even rather toxic drugs are sometimes used instead.
The emergence of drug-resistant fungal strains is also a growing threat. Of great concern is the rise in multi-drug resistant Candida species, azole-resistant Aspergillus species and clinically resistant Cryptococcus.
Management strategies
Fungal threats are adding pressure to overburdened health systems with a limited arsenal of treatment options.
Healthcare professionals, scientific researchers, policymakers and governments must address the gaps in the diagnosis and management of fungal infections. This will help to improve capacity to deal with them.
Rachael Dangarembizi, Neuroinfections Researcher, Division of Physiological Sciences, University of Cape Town
This article is republished from The Conversation under a Creative Commons license. Read the original article.