Chronic binge drinking may prematurely age your brain
In a recent publication in the Journal of Neurovirology (March 2022) UCT researchers set out to test the hypothesis that HIV infection and heavy binge drinking will be associated with premature ageing of the brain.
Not only does South Africa have the highest number of people with HIV in the world, but it also has one of the highest rates of binge drinking (particularly amongst men), says Ipser, lead author on the paper. Both clinical and animal research indicates that heavy alcohol use in HIV patients is associated with poorer treatment adherence, greater immunosuppression, elevated risk of opportunistic infections, higher rates of TB, and more rapid mortality, says Ipser. And so, estimates that as many as one third of HIV positive patients attending clinics in Cape Town engage in hazardous drinking behaviour underscores just how dire the public health consequences of comorbid HIV and heavy drinking are likely to be.
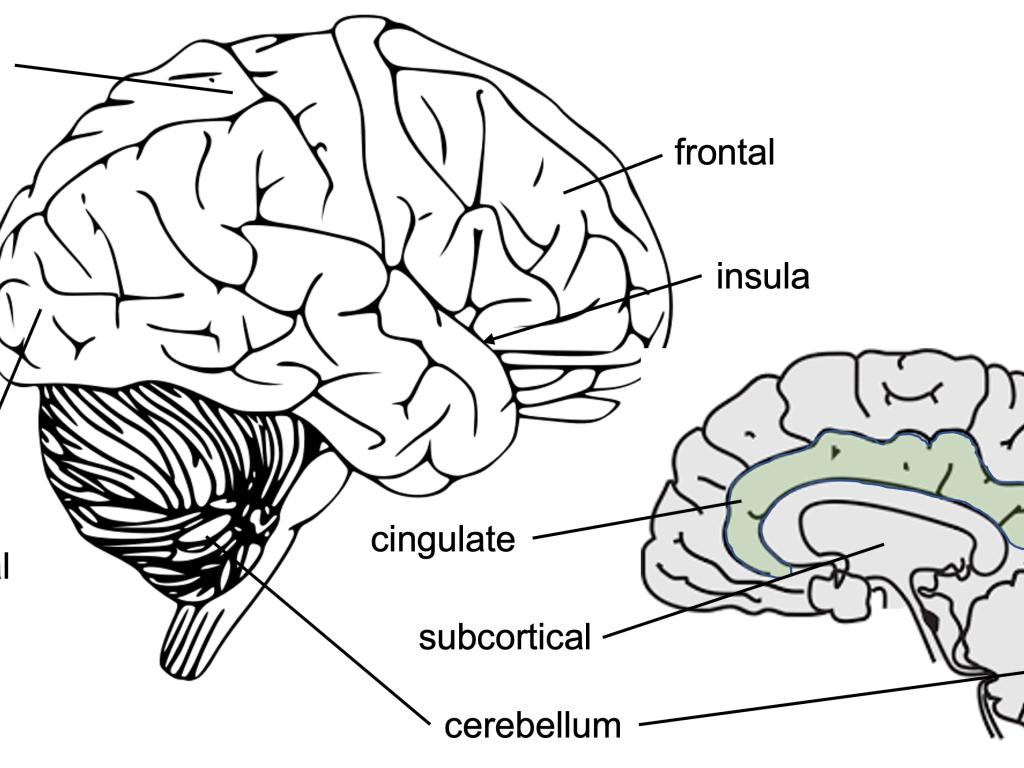
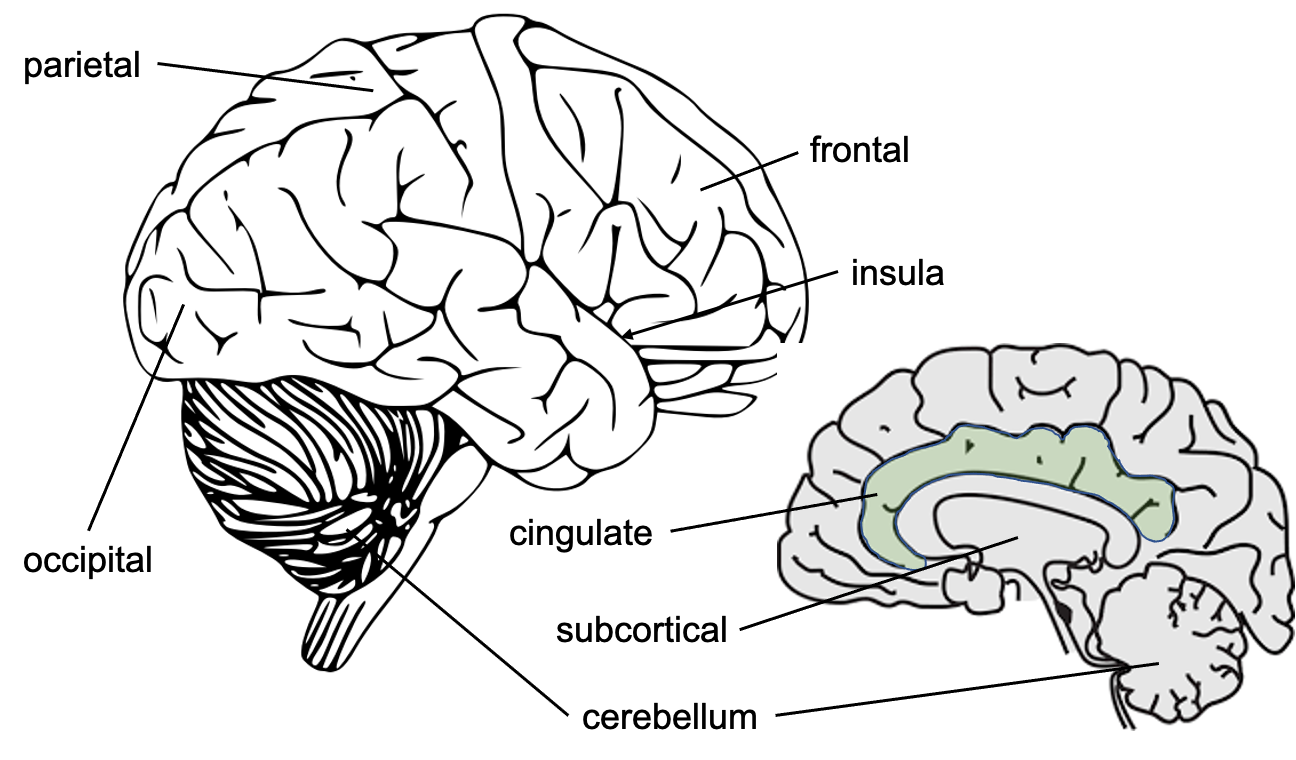
In this study a machine-learning model was applied that had been trained to estimate brain age based on 1118 features extracted from brain MRI scans, including cortical thickness, surface area, and subcortical/cerebellar volumes to a group of people with HIV, and healthy controls recruited from a community health clinic in Khayelitsha. HIV positive and negative participants were in turn divided into heavy drinkers and light drinkers. The ‘brain age gap’ - an output measure of how old the algorithm estimates your brain to be minus your actual chronological age - was used in this study to compare heavy drinkers to light drinkers and those with HIV to those without. The higher the brain age gap the worse off you are.
Heavy binge drinking was defined as people consuming 6 standard drinks per occasion at least once a week during the past year. Light drinking was defined as people consuming at least one drink over the past year, who drank at most 2 to 3 times a week, but who did not drink more than 2 drinks on a typical day during the previous year. Sixty-nine participants were recruited into the study. Neurocognitive tests and MRI scans were performed and HIV viral load and CD4 count were measured.
The main finding of this study was that heavy binge drinking was associated with substantially greater ageing of the brain. Amongst HIV negative participants, brains of heavy drinkers on average looked like those of light drinkers more than 8 years their senior. Although this study did not find a statistically significant association between HIV status and advanced brain ageing, contradicting previous reports, a relatively large effect size for HIV suggests that the study may not have had sufficient power to detect an association. A well-powered analysis using the same brain age model in a large (N > 1,500), multi-site, global cohort from the ENIGMA consortium is currently planned that should address this limitation.
This particular brain age model was developed by Tobias Kaufmann at the Norwegian Centre for Mental Disorders Research (NORMENT). Ipser visited NORMENT in 2019 for a couple of weeks, as part of an ongoing research collaboration between the Psychiatry Dept at UCT and NORMENT, during which time he received training in applying Kaufmann's model. The benefit of the Kaufmann model is that it has been trained on a very large sample of MRI scans (35,474 from healthy individuals) and covers a very wide age range (3-89 years). It has also previously demonstrated efficacy in discriminating between specific psychiatric populations, both with respect to global brain age, as well as models trained on specific brain regions (occipital, frontal, temporal, parietal, cingulate, insula, and subcortical/cerebellar regions). Indeed, in this paper, advanced brain age in heavy binge drinkers was particularly apparent in the parietal, cingulate and subcortical regions of the brain. This is important because the brain ages differentially depending on the area, whereas the majority of models only give a global age, and that is where the Kaufmann model is particularly powerful.
However, as with most models it has been trained almost exclusively with individuals living in high income countries, since these populations have a higher socioeconomic status than populations from low- and middle income countries such as South Africa this may account for the brain age gap of approximately 5 years apparent in the control group, where we would expect none. It’s possible that poorer nutrition, toxins and other negative environmental factors in low- and middle-income countries may account for brain ageing effects compared to a high-income cohort. It is hoped that initiatives such as the Neuroscience Institute’s African Brain Health Genomics Project will enable the training of brain age models that are more representative of populations living in our context.
This kind of technology enables the analysis of a huge amount of data to be done in parallel and, from a statistical point of view, means you don’t need to correct for multiple comparisons, which is an incredible strength. Furthermore, calculating brain age gap is particularly nice because the resulting metric is a single number and is fairly intuitive.
The field of brain ageing using machine learning is still relatively immature, and there is little consensus on exactly what greater brain age actually means, particularly when measured at the level of an individual patient. However, what the use of this technology makes particularly clear in this paper is that the association between heavy binge drinking and brain age gap, independent of HIV status, points to the importance of screening for alcohol use disorders in primary care.
Original journal article: Ipser J.C., Joska J., Sevenoaks T., Gouse H., Freeman C., Kaufmann T., Andreassen O.A., Shoptaw S., Stein D.J. (2022). Limited evidence for a moderating effect of HIV status on brain age in heavy episodic drinkers. J Neurovirol 1–9, doi:10.1007/s13365-022-01072-5.
https://pubmed.ncbi.nlm.nih.gov/35355213/