Why won’t it stop? Understanding treatment-resistant epilepsy

UCT Neuroscience Institute researcher Joseph Raimondo and former student Richard Burman together with clinician researcher Jo Wilmshurst just landed a review in the prestigious Nature Reviews Neurology entitled: ‘Why won’t it stop? The dynamics of benzodiazepine resistance in status epilepticus.’ Status epilepticus is a state of persistent seizure activity that lasts for more than 5 minutes and is a neurological emergency that can be life threatening. Currently the benzodiazepine class of drugs are the first-line treatment for status epilepticus, however they don’t always work, and it is important to understand why.
This important review and meta-analysis explores the state of benzodiazepine-treatment resistance in low and middle-income countries (LMICs) where drug resistance rates are higher than in high-income countries (HICs). The neurological events following status epilepticus can be severe, leaving individuals impaired, disabled and ostracized by their communities and society. Figure 1a shows that the average incidence of status epilepticus and benzodiazepine resistance is approximately 45% for LMICs and 28% for HICs. It is clear that the social and economic impact of this problem is huge and that LMICs are bearing the brunt of this burden, but why?
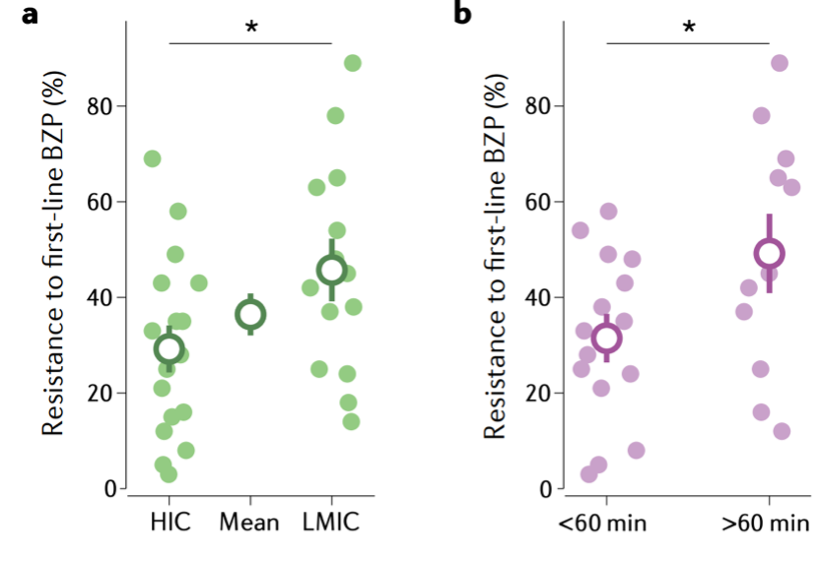
It turns out that treatment resistance is an issue of time to treatment! Evidence suggests that long episodes of status epilepticus alter brain physiology, thereby contributing to the emergence of benzodiazepine resistance. Such changes include alterations in GABAA receptor function and in the transmembrane gradient for chloride, both of which erode the ability of benzodiazepines to bring the seizures to an end.
Current clinical management guidelines for status epilepticus seldom account for these duration-related changes in brain physiology, having significant implications for the treatment of individuals in LMICs, where the average time taken to reach medical attention is longer than in HICs. In this perspective article, Burman et al combine clinical insights and the latest evidence from neuroscience to inspire a new, context-specific, best practice approach to managing status epilepticus. The authors are made up of scientists and medical specialists and as such they aim to ‘address the issues from bench (lab) to clinic (bedside)’ says co-author Jo Wilmshurst.
Patients in under-resourced settings often present at their nearest clinic in a state of prolonged seizure, and since time-since-onset of seizure should be considered a critical factor in predicting benzodiazepine resistance, combination therapy should be considered much earlier in such cases.
Furthermore, an understanding of the cellular and molecular mechanisms underlying benzodiazepine resistance gleaned from experimental studies should inform the optimization of future strategies for managing status epilepticus.Raimondo
"We are excited by the possibility that our research in this area could help improve the treatment of patients in status epilepticus," says Joseph Raimondo